If you are a primary care provider and still wondering whether to provide Chronic Care Management (CCM) or not, then you need to act quickly in 2025. With over 70% of the US adults living with at least one chronic condition, primary care practices are now long-term coordinators of care.
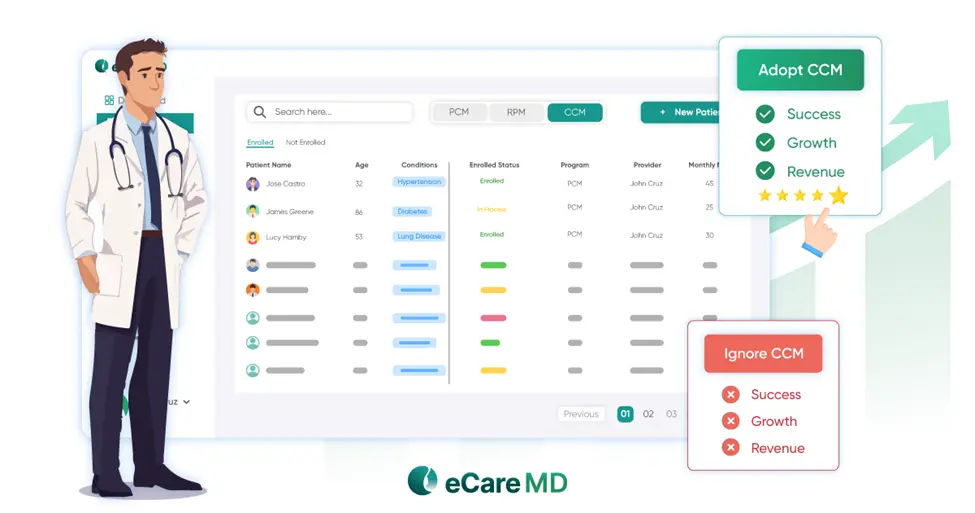
This is not the time to sit on the fence, as you are missing out on an opportunity to improve outcomes and revenue by leveraging CCM. And with value-based care becoming the core of healthcare, instead of the quantity of services, quality is more important.
Moreover, the barriers like low staff, care coordination challenges, patient engagement, and reimbursement challenges can now easily be overcome with modern CCM software. Even small independent practices can deliver continuous, coordinated care.
Plus, with features like automated time tracking, virtual check-ins, and built-in compliance support, you don’t have to worry about documentation errors or extra work.
This is why, in this blog, we will discuss exactly why CCM is no longer optional in 2025 and how the right chronic care management software can set your practice up for long-term success.
So, let’s get started without any ado!
The Changing Healthcare Landscape: Market Forces Driving CCM Adoption
With nearly 50% of Medicare payments shifting to value-based care models and CCM at the center, it’s no wonder that CCM is gaining traction. This is just not the changing of policies; it’s about missing an opportunity to earn quality bonus payments and risk falling behind in the race for value-based contracts.
Moreover, it’s not just the payers like Medicare; patients also want coordinated care. Plus, the chronic care management platform is now becoming a benchmark for patients who want coordinated care.
The Centers for Medicare and Medicaid Services (CMS) is also continuously expanding reimbursement rates and broadening qualifying conditions. However, the catch is that compliance requirements are going up with benefits. That’s why CCM software is becoming more than just a nice-to-have; it’s becoming mandatory for better managing care coordination and regulatory compliance.
Finally, competition is becoming more aggressive, and remaining passive without adopting the CCM program is no longer an option. The only way small and mid-sized practices can stay competitive is by investing in patient care management software that allows smooth delivery of coordinated care without overburdening the staff.
Long story short, in 2025, the healthcare market is moving towards value-based coordinated care, and CCM is irreplaceable to stay in the competition. So, let’s see what financial benefits a primary care provider can reap from CCM.
The Financial Opportunity: Revenue Potential & Practice Sustainability
Although CCM is there to improve the quality of care for chronic patients, it is also a revenue generator for care providers. For instance, in 2025, Medicare reimburses $43.92 for CPT code 99490 and $94.32 for CPT code 99491 per patient per month.
This adds up quickly, and with the right primary care CCM platform, even a modest patient panel can earn additional revenue without adding extra staff. You can further boost this by adding Remote Patient Monitoring (RPM) with integrated CCM software, and you can earn an additional $62 to $89 per patient per month.
Adopting CCM is not only about earning extra income but also about sustainability. With CCM, the chances of patients staying with your practice increase tremendously. The reason for this is that care management systems keep them engaged, supported, and connected.
In addition to this, operations are also streamlined as proactive care reduces emergency visits and hospitalizations significantly. And when combined with patient care management software automation, you are looking at thousands of dollars saved in administrative costs. Add smarter workflows to the mix, and you’ve got a more efficient staff and better productivity right there.
Finally, you can claim all value-based bonuses. CCM boosts MIPS quality score, qualifies you for Medicare Advantage incentives, and helps you tap into ACO shared savings. In short, CCM opens multiple revenue streams for you, boosting your finances.
The Cost of Inaction: What Practices Risk by Waiting
When you stall on whether or not to bring CCM into your primary care, then you are putting the future of your practice on the line. This may sound exaggerated, but it’s not, as patients are no longer looking at only the reputation or location of a care facility.
They now want comprehensive care coordination and patient care management software, and if you lack these, you’re automatically at a disadvantage. Then comes the financial toll, as fee-for-service is being overtaken by value-based care bonuses.
Moreover, practices without the CCM software are unable to leverage these bonuses or high-value contracts. This is why the longer you wait, the more you are losing the opportunity to monetize these revenue options.
CMS is also tightening the regulations and making CCM a cornerstone of quality reporting and reimbursement eligibility. Without primary care chronic care management software, you might be excluded from programs you depend on for revenue generation.
At last, your team also needs help from a primary care CCM software that automates routine and repetitive tasks. This relieves them of extra work and allows them to focus on patient care rather than handling the paperwork.
In short, not acting now will not only negatively impact your finances but also your reputation and future growth.
Technology Enablement: How Modern CCM Software Makes Implementation Feasible
Many providers think that implementing CCM software will take forever, and their care delivery will be interrupted. But the reality is that today’s chronic care management software is built for speed; this is why most CCM platforms can be operational within 30 to 60 days.
Furthermore, with pre-built templates and workflows, you don’t need to invest in customizations. Plus, with cloud-based deployment, you need minimal IT setup with no servers and no complex tech. Modern care management software swiftly integrates with existing EHRs and practice management tools, keeping the data flow seamless.
Another advantage is that everything from patient identification and enrollment to care plan generation and time tracking can be automated. With CMS guidelines built right into the platform, you are always compliant and reimbursed fully.
Scaling also becomes easy as you can shift from 50 patients to 500+ patients with the same patient care management software. These platforms are designed to accommodate various practice sizes with flexible pricing models and scalable infrastructure. You can also add telehealth, RPM, and predictive analytics later on and expand your services.
Finally, if you fear how to train staff with the software, then don’t worry, as leading vendors provide staff training. They also offer ongoing support and dedicated implementation teams to ensure your software functions as it should.
Implementation Strategy for 2025: Getting Started & Scaling Success
To ensure successful implementation, you need to start slow instead of going all in. So, first, do a pilot test with a small number of patients; this will give you an idea of the issues and help you fix them early. Next, train your staff to use the CCM software properly and make sure they understand all the functions and benefits of the platform.
If you think that a big budget is needed to launch CCM, then that’s not true. But even if you invest big, you can recover most of the amount within four to eight months and start earning a profit. Moreover, if you enquire, many vendors would offer flexible pricing and financing models.
Finally, patient buy-in is crucial. Explain the benefits and their advantages by enrolling in CCM in plain language without adding much technicality. Also, ensure that you market yourself as a comprehensive chronic care provider to improve visibility and trust, as well as boost retention.
Here’s a table that explains the steps to take in short form, so you understand everything clearly and quickly:
| Strategy Area | Action Step |
| Pilot Program | Start with 50–100 high-risk patients and track ROI |
| Staff Training | Use vendor-provided training and build team confidence with phased adoption |
| Financial Planning | Leverage flexible pricing, estimate ROI in 4–8 months, and explore grant options |
| Patient Communication | Educate patients using CCM tools, update marketing to highlight care coordination |
By following this approach, you can roll out CCM without disrupting your practice and scale it into a reliable, revenue-generating care model.
Conclusion
Ignoring Chronic Care Management (CCM) in 2025 is not just risky, it’s a missed opportunity for growth, better care, and financial sustainability. For that, you require the right CCM software for primary care practices, and even small practices can deliver coordinated care, boost patient outcomes, and tap into new revenue streams.
So, ready to thrive in today’s competitive and value-based healthcare? Click here to make CCM your practice’s competitive edge today.
Frequently Asked Questions
- What is the minimum patient volume needed for a primary care practice to justify implementing CCM?
Chronic care in primary care practice can justify implementing CCM with as few as 50 to 100 eligible chronic care patients. That’s often enough to see meaningful ROI, especially with the help of CCM software that automates workflows and billing, making it manageable even for smaller teams.
- How quickly can primary care practices see ROI from CCM program implementation?
Primary care practices can typically see a return on investment from their CCM program within 4 to 8 months. Thanks to recurring monthly reimbursements, streamlined workflows, and reduced administrative load, small practices notice financial and operational benefits fairly quickly after implementation.
- What are the biggest barriers primary care practices face when starting CCM programs?
One of the biggest hurdles for primary care practices starting CCM is feeling overwhelmed, limited staff, lack of time, and uncertainty about compliance often hold them back. Many also worry about workflow disruptions and upfront costs, even though modern CCM software can ease these concerns.
- How does CCM integration affect existing primary care workflows and staff responsibilities?
Integrating CCM into primary care workflows actually lightens the load. With automation handling time tracking, documentation, and care plan updates, staff can focus more on patient care and less on paperwork. It streamlines tasks, reduces burnout, and makes care coordination feel more manageable, not more overwhelming.
- What CMS requirements must primary care practices meet for CCM billing in 2025?
To bill for CCM in 2025, primary care practices must meet CMS requirements, such as having patient consent, creating a comprehensive care plan, delivering at least 20 minutes of non-face-to-face care monthly, and documenting everything properly. Plus, time tracking and using certified EHRs are now essential for compliance.
- How can small primary care practices compete with large health systems in CCM delivery?
Small primary care practices can compete using modern CCM software that levels the playing field. With features like automation, care plan templates, and EHR integration, they can deliver the same high-quality, coordinated care without needing a large staff or complex infrastructure. It’s smart, scalable care.
Also Read-Stay Healthy as a Gamer: How to Prioritize Your Health as a Gamer?